Understanding Hereditary Persistence of Foetal Haemoglobin (HPFH)
- EJB
- Apr 26, 2025
- 3 min read
Hereditary Persistence of Foetal Haemoglobin (HPFH) is a fascinating genetic condition that has significant clinical implications. While it is often asymptomatic, its interaction with other blood disorders can greatly influence disease severity and patient outcomes. In this article, we will explore what HPFH is, its causes, types, and why understanding this condition is important.

What is Foetal Haemoglobin?
Foetal haemoglobin (HbF) is the main type of haemoglobin produced by a developing baby in the womb. It has a stronger affinity for oxygen than adult haemoglobin, allowing an efficient transfer of oxygen from the mother's bloodstream to the foetus. Normally, after birth, the production of HbF decreases rapidly and is replaced by adult haemoglobin (HbA).
However, in some individuals, the production of HbF continues into adulthood. When this occurs due to inherited genetic traits, it is referred to as Hereditary Persistence of Foetal Haemoglobin.
What Causes Hereditary Persistence of Foetal Haemoglobin?
HPFH is caused by mutations in the regulatory regions of the β-globin gene cluster located on chromosome 11. These mutations prevent the normal switch from foetal to adult haemoglobin production. As a result, individuals maintain higher levels of HbF throughout their lives.
There are two primary forms of HPFH:
Deletional HPFH: Large segments of DNA are deleted near the β-globin gene cluster, leading to continued production of HbF.
Non-deletional HPFH: Point mutations or small changes in the DNA sequence alter the regulation of haemoglobin switching without large deletions.
Both forms are inherited in an autosomal dominant manner, meaning that inheriting just one copy of the mutated gene from a parent can result in HPFH.
Symptoms and Diagnosis
Interestingly, individuals with HPFH typically experience no symptoms and lead normal lives. The condition is usually discovered incidentally during routine blood tests that show elevated levels of HbF. HPFH can be confirmed through:
Haemoglobin electrophoresis: A laboratory technique that separates different types of haemoglobin.
Genetic testing: Identifying specific mutations in the β-globin gene cluster.
In some cases, HPFH is distinguished from similar conditions such as β-thalassaemia trait by careful analysis of red blood cell indices and haemoglobin patterns.
Clinical Significance
While HPFH alone does not cause health problems, it can have a significant impact when inherited alongside other haemoglobin disorders. For example:
Sickle Cell Disease: Individuals with sickle cell disease and co-existing HPFH often have milder symptoms because the elevated levels of HbF inhibit the sickling of red blood cells.
β-thalassaemia: HPFH can reduce the severity of β-thalassaemia by partially compensating for defective adult haemoglobin production.
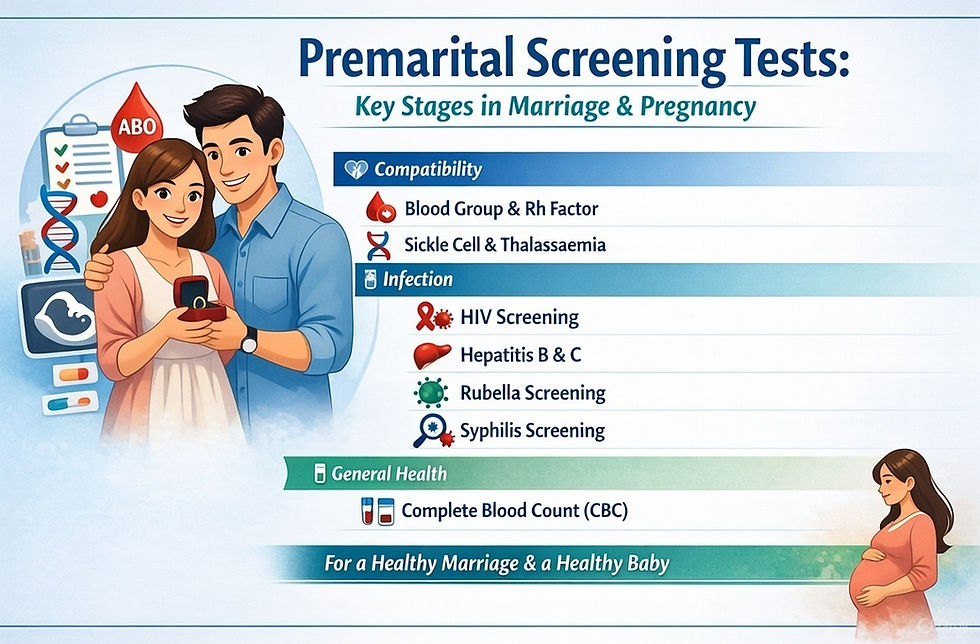
Therefore, recognising HPFH can be crucial in genetic counselling and managing related haemoglobinopathies.
Management and Outlook
Since HPFH does not typically cause any health issues, no treatment is necessary. However, individuals with HPFH who are planning to have children may wish to undergo genetic counselling, especially if their partner also carries a haemoglobin disorder. In cases where HPFH modifies the clinical presentation of other conditions, medical monitoring may be advised.
The outlook for individuals with HPFH is excellent. They usually enjoy a normal life expectancy and do not require any medical intervention related to their haemoglobin levels.
Conclusion
Hereditary Persistence of Foetal Haemoglobin is a benign genetic trait that highlights the complexity and beauty of human biology. While it is generally harmless on its own, understanding HPFH is essential, particularly in the context of other haemoglobin disorders. Awareness of this condition can lead to better diagnosis, improved patient management, and more informed genetic counselling.
If you have questions about your haemoglobin levels or have a family history of blood disorders, it is advisable to seek guidance from a healthcare professional or a genetic counsellor.



Comments